Your results indicate that you have symptoms commonly associated with pelvic organ prolapse.
Instead of living with POP, live better without it.
Thank you for completing this self-assessment. Based on your answers you have symptoms commonly associated with pelvic organ prolapse.
If you haven’t already, you may want to talk with a doctor about your symptoms and potentially start discussing what treatment options would be right for you. We have a Physician Finder directory with specialists who can treat POP and other pelvic floor disorders.
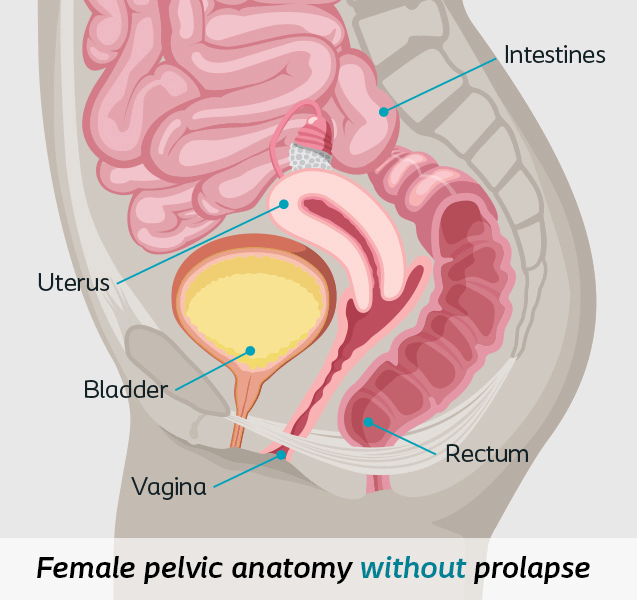
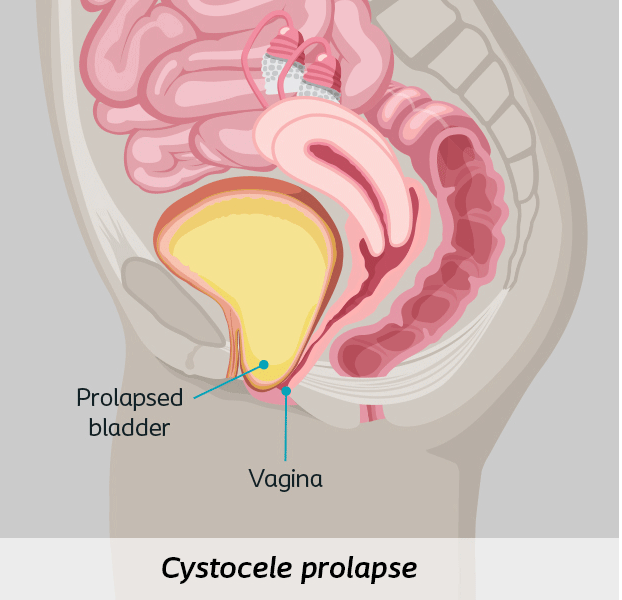
What is prolapse?
Up to 50% of women will experience pelvic organ prolapse.1
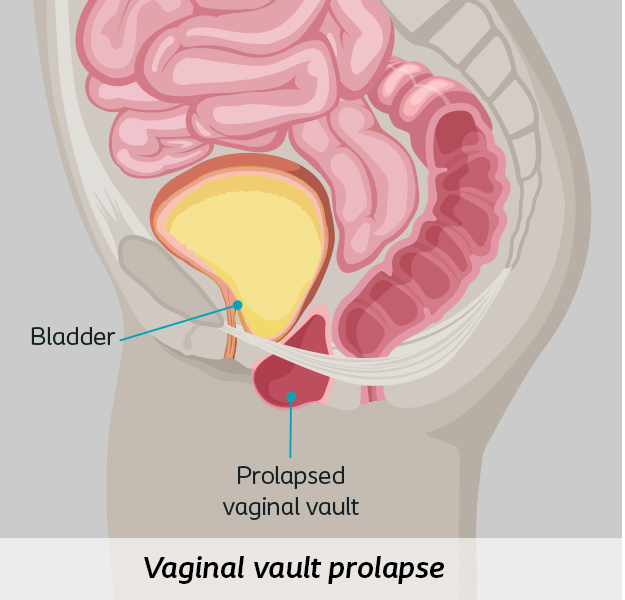
Pelvic organ prolapse (POP) is the dropping of the pelvic organs caused by the loss of normal support of the vagina. It occurs when there is weakness or damage to the normal support of the pelvic floor causing pelvic organs (the vagina, cervix, uterus, bladder, urethra, intestines or rectum) to drop down. Women with POP may feel or see a bulge coming out of the opening of their vagina.2
Symptoms of prolapse
While it is not life-threatening, women with prolapse experience symptoms that impact their day-to-day lives and keep them from experiencing moments to the fullest. But these symptoms won’t always seem obvious. As prolapse progresses, the symptoms may become more apparent and painful. If you are experiencing prolapse, you may feel:
- Pressure in the pelvic region, vaginal discomfort, pain or bleeding3
- Pulling or aching in the lower abdomen or pelvis, a bulge coming out of the vagina3
- Pain or discomfort during sex4
- Difficulty urinating or having a bowel movement3
Symptoms of prolapse
While it is not life-threatening, women with prolapse experience symptoms that impact their day-to-day lives and keep them from experiencing moments to the fullest. But these symptoms won’t always seem obvious. As prolapse progresses, the symptoms may become more apparent and painful. If you are experiencing prolapse, you may feel:
- Pressure in the pelvic region, vaginal discomfort, pain or bleeding3
- Pulling or aching in the lower abdomen or pelvis, a bulge coming out of the vagina3
- Pain or discomfort during sex4
- Difficulty urinating or having a bowel movement3
What causes prolapse?
Pelvic organ prolapse can drastically impact your lifestyle. Things that can cause the muscles in the pelvis to become stretched or weakened include:
- Pregnancy and childbirth2
- Genetics2
- Smoking2
- Pelvic Floor Injury2
- Chronic constipation2
- Chronic coughing2
- Obesity2
- Menopause2
- Nerve and muscle diseases2
What causes prolapse?
Pelvic organ prolapse can drastically impact your lifestyle. Things that can cause the muscles in the pelvis to become stretched or weakened include:
- Pregnancy and childbirth2
- Genetics2
- Smoking2
- Pelvic Floor Injury2
- Chronic constipation2
- Chronic coughing2
- Obesity2
- Menopause2
- Nerve and muscle diseases2
Locate a pelvic health specialist near you
Simply enter your ZIP code to see a listing of pelvic doctors in your area. Each listing provides the doctor’s name and area of pelvic health expertise, along with their website, phone number and distance from your home.
This directory was created and is maintained by Coloplast. It is intended to support patients who want to learn more about treatment options for stress urinary incontinence (SUI) and pelvic organ prolapse (POP) by helping connect them to physicians who have demonstrated qualifications and interest in providing quality care for these conditions. Names and details in this directory are provided for your information only. Decisions regarding choice of physician and treatment are a patient’s responsibility, as is all communication and interaction with listed medical professionals. Any information you send to a physician is not covered by the Coloplast Privacy Policy.
Physicians listed on the Physician Locator pay no fee for inclusion. Some physicians on this list may purchase products from, provide consulting services to and/or be a party to a co-marketing agreement with Coloplast. Coloplast makes no representations or warranties regarding, and shall not be responsible for, the competencies or skill level of any of the physicians listed on the Physician Locator or the quality of their procedural outcomes. You and your physician must determine the right procedure for you.
For more information about this physician finder or if you have questions about how to add or manage directory listings please contact the administrator.